In recent years, healthcare has undergone a transformation that’s reshaping how providers care for patients with chronic diseases. One of the most impactful changes has been the widespread adoption of remote patient monitoring (RPM). With the rise of wearable technologies, mobile health apps, and telehealth platforms, patients are now able to manage their health conditions from the comfort of their homes — while still staying connected to their care teams. This shift has created new possibilities for improving outcomes, increasing access, and reducing healthcare costs.
What Is Remote Patient Monitoring?
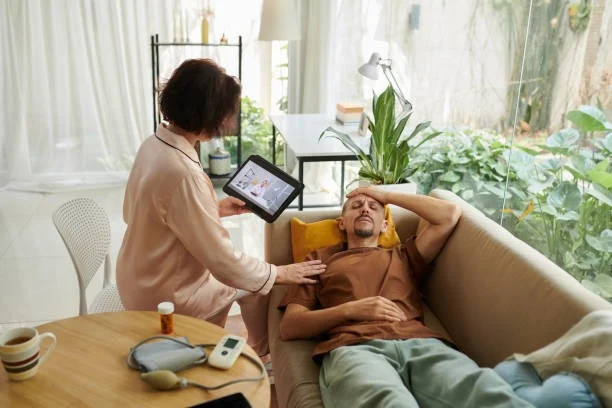
Remote patient monitoring refers to the use of digital technologies to track patients’ health data outside of traditional clinical settings. Common tools include blood pressure cuffs, glucose meters, heart rate monitors, and wearable fitness trackers. These devices collect real-time data that is then securely transmitted to healthcare providers, allowing for continuous monitoring and timely intervention.
For individuals managing chronic illnesses such as diabetes, hypertension, or heart disease, RPM offers a convenient and proactive way to stay on top of their health. Rather than waiting for symptoms to worsen or relying solely on periodic check-ups, patients and providers can make informed decisions based on real-time insights.
Chronic Disease and the Need for Ongoing Support
Chronic conditions require long-term care strategies. Traditionally, patients with these conditions face frequent doctor’s visits, long drives to appointments, and high out-of-pocket expenses. These challenges are even more pronounced in rural communities where access to specialty care may be limited.
Remote monitoring helps fill these gaps. For instance, a patient with congestive heart failure can use a digital scale and blood pressure monitor at home, with results reviewed daily by a nurse or physician. Any concerning changes can trigger early interventions, potentially avoiding hospitalizations and worsening symptoms.
This continuous care model improves adherence to treatment plans and builds trust between patients and providers. It also helps individuals feel empowered and engaged in their own care — a key factor in long-term health management.
Advantages of RPM for Providers and Patients
The benefits of RPM are far-reaching. From the provider’s perspective, having access to real-time health data can lead to more personalized care plans and faster adjustments to medications or treatments. This kind of responsiveness can significantly improve patient outcomes.
For patients, RPM provides flexibility, reduces unnecessary visits, and increases peace of mind. It also encourages accountability, as many devices offer reminders and feedback that keep users engaged in healthy behaviors.
In the broader system, RPM can lead to lower healthcare costs. Fewer emergency room visits, shorter hospital stays, and improved chronic disease management all contribute to financial savings — especially for public programs like Medicare and Medicaid.
Overcoming Barriers to Implementation
Despite its benefits, RPM adoption still faces hurdles. The digital divide remains a significant concern, particularly in rural and underserved areas. Many patients may lack reliable internet access or feel uncomfortable using technology. Training, education, and community-based support are essential to closing this gap.
Reimbursement is another challenge. While policy changes have expanded coverage for RPM services, especially during the COVID-19 pandemic, there’s still a need for consistent and sustainable payment models to support long-term implementation.
Healthcare organizations must also address data privacy and security. Protecting sensitive patient information requires robust cybersecurity measures and adherence to federal regulations.
Real-World Success Stories
Across the country, healthcare systems are seeing success with RPM programs. In Mississippi, a remote monitoring initiative for diabetes patients led to significant reductions in A1C levels and emergency room visits. In New York, RPM helped reduce readmission rates among heart failure patients by nearly 50%.
Lena Esmail, a healthcare leader and advocate for accessible care, has seen firsthand how RPM can transform outcomes in rural and underserved communities. Her organization has implemented remote monitoring tools to help patients manage chronic illnesses with greater ease and efficiency. Lena Esmail believes these models are the future of chronic care management, especially in areas where traditional access is limited.
A Future Built on Connection
The rise of remote patient monitoring is not just a trend — it’s a paradigm shift in how healthcare is delivered and experienced. As technology continues to advance, we can expect RPM to become even more integrated into primary care and chronic disease management.
To truly harness its potential, we must ensure that all communities — regardless of income, geography, or background — have access to the tools and support they need. By doing so, we can create a more equitable, connected, and patient-centered healthcare system that meets people where they are.
Remote patient monitoring is more than a convenience — it’s a lifeline for those living with chronic disease. With thoughtful implementation and a commitment to health equity, it can be the key to healthier lives at home and beyond.

Lexy Summer is a talented writer with a deep passion for the art of language and storytelling. With a background in editing and content creation, Lexy has honed her skills in crafting clear, engaging, and grammatically flawless writing.